Preamble
The most common type of corneal ectasia, keratoconus presents in adolescence and stabilizes during the third or fourth decade of adulthood. Patients can suffer mild to severe visual impairment from irregular astigmatism, myopia, vertical coma, or corneal scarring. Management begins with spectacles, often progresses to rigid gas permeable (RGP) contact lenses, and may advance to corneal transplantation if the patient cannot tolerate the lenses or see adequately with them. Some 10% to 20% of patients require corneal transplant surgery.
Keratoconus affects individuals of all biological sexes and all ethnicities. Patients present with blurred vision due to irregular astigmatism and/or coma, the most common higher-order aberration in this population. They often report decreased vision with spectacles and major changes in refraction that lead them to replace spectacles within a year of their last prescription.
Keratoconus is characterised by progressive corneal thinning with resultant irregular astigmatism and myopia. Its prevalence has been estimated at 1:375 to 1:2000 people globally, with a considerably higher rate in the younger populations.
Over the past two decades, our global initiative to help people become more involved in the important decisions about their life's and it becoming a lifeline that caused a paradigm shift in the management of keratoconus. The treatment has expanded significantly from conservative management (e.g., spectacles and contact lenses wear) and penetrating keratoplasty to many other therapeutic and refractive modalities, including corneal cross-linking (with various protocols/techniques), combined CXL-keratorefractive surgeries, intracorneal ring segments (CAIRS, INTACS), anterior lamellar keratoplasty, and more recently, bowman’s layer transplantation, stromal keratophakia, and stromal regeneration.
Rapid Deployment and Unity
Several recent large genome-wide-association-studies (GWAS) have identified important genetic mutations relevant to keratoconus, facilitating the development of potential gene therapy targeting keratoconus and halting the disease progression. In addition, attempts have been made to leverage the power of artificial intelligence-assisted algorithms in enabling earlier detection and progression prediction in keratoconus.
In this guide, we provide an overview of the Keratoconus landscape and of the new syngeneic (co) management of this common clinical entity.
Classifying the Condition
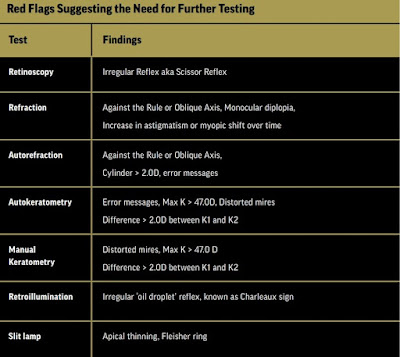
Optometrists are often the first clinicians to interact with and with referring patients to an Ophthalmologist for further testing to confirm diagnosis of Keratoconus suspected patients. A treatment or a treatment plan can only begin once a diagnosis has been made of those suspected of having Keratoconus. Corneal topography is the primary diagnostic tool. The classic presentation is central or inferior steepening and thinning. Findings suggestive of keratoconus include astigmatism greater than 5 diopters (D), maximum keratometry readings greater than 49 D, and central corneal thickness of less than 470 µm.
Both the Amsler-Krumeich classification method (which measures degree of refractive error, average anterior corneal curvature, corneal thickness at the thinnest location, and presence of scarring) and the Belin ABCD grading system (which analyses anterior and posterior radius of curvature, thinnest corneal thickness, and best corrected distance visual acuity) can be used to categorize disease severity. Scheimpflug tomography can also be used to examine the posterior surface of the cornea, which is often affected in keratoconus, and to detect early ectasia. Later stages of the condition will show anterior and posterior steepening.
Mild: Spectacles, Soft Lenses, CXL
Depending on severity, different options exist for the management of keratoconus. In the early stages, patients can use spectacles or soft contact lenses. Soft toric contact lenses are not often used because they do not address irregular astigmatism or higher-order aberrations. And although more custom options are available, such as lathed-cut soft lenses with quadrant-specific capabilities and greater central thickness, they too suffer from the same limitations. In general, soft lenses are used in milder forms of keratoconus or when the patient is unable to tolerate gas permeable (GP) lenses. Lens selection also depends on patient lifestyle and ability to care for the devices.
At initial diagnosis, corneal collagen crosslinking (CXL) should be considered because it halts disease progression and increases the cornea’s biomechanical properties, strengthening and stabilizing the collagen lamellae and promoting the formation of collagen bonds that stiffen the cornea, a process that occurs naturally with age.
According to the Dresden protocol (the conventional CXL method), the central 7 to 9 mm of the corneal epithelium should be removed and the cornea soaked with a solution of 0.1% riboflavin-5-phosphate and 20% dextran every 5 minutes for a total of 30 and subsequently exposed to UVA radiation (370 nm, 3 mW/cm2) for another 30 minutes. Accelerated versions of the procedure can protect the deepithelialized cornea from infection and increase both patient comfort and treatment efficacy. There is also a transepithelial (epi-on) version of the procedure that is less painful and decreases the risk of complications caused by removing the epithelium. Traditional (epi-off) CXL, however, has been shown to result in a more regular corneal surface.
Optimization of the parameters continues with newer epi-off crosslinking protocols showing promise in efficacy, in patient comfort, in reducing treatment time and in optimizing safety.
CXL is indicated in patients whose Keratoconus progresses. There are a variety of different markers that can be used to measure progression, some of which include: an increase in anterior or posterior corneal curvature, change in manifest refraction, or decrease in corneal thickness. It is also recommended in young patients diagnosed at an early age and thus most likely to progress given that paediatric keratoconus often advances at a faster rate. These patients should consider undergoing CXL before significant progression has been observed.
Standard CXL is contraindicated if corneal thickness is less than 400 µm, however there are protocols available to address this issue (to avoid UVA damage to the posterior cornea, anterior chamber, lens, and retina), if corneal scarring is present, or if there is prior/active herpetic eye infection. Patients who wore contact lenses before CXL will generally have to resume wearing them after the procedure. The success of CXL, which decreases the need for corneal transplantation, highlights the importance of early diagnosis, close monitoring, and prompt referrals.
Moderate: CAIRs, PRK, ICRSs, RGP lenses, Hybrid Lenses, Piggybacking
Intracorneal ring segments (ICRSs) are made of polymethyl methacrylate and have an arc-shortening effect, thus altering the corneal lamellae and flattening the central cornea. They can be implanted during or before CXL and can be subsequently removed if needed. ICRSs may increase difficultly in fitting contact lenses because the entire cornea and ICRSs must be vaulted.
Relatively new tissue implants, often referred to as 'CAIRS' (Corneal Allogenic Intrastromal Ring Segments), are being used to solve many of the limitations which came with ICRS. Also for some patients 'CTAK' (Cornea Tissue Addition Keratoplasty), which involves placing a custom tissue in-lay into the cornea which has protocols that differ to 'CAIRS', as well as 'doughnut lenticule implants,' and also limited customized topography guided surface ablation (of which the most widely known is the 'Athens Protocol'), in combination with CXL, may also be options depending on the patient case. Read more...
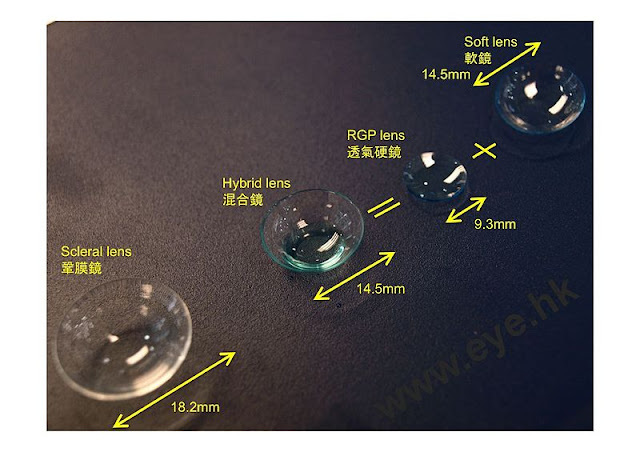
RGP lenses - which allow for the tear exchange between cornea and lens that neutralizes irregular astigmatism - are the mainstay of corrective treatment for mildly to moderately conical corneas. Other options are the hybrid (RGP centre surrounded by a soft lens skirt) and piggybacking (RGP lens atop soft lens) systems. Both combine the benefits of soft and rigid lenses and may be used to address poor adaptation to RGP lenses and lens decentration and ejection.
Severe: Scleral Lenses, Corneal Transplant
Scleral contact lenses (ScCLs) are RGP lenses whose diameter is larger, usually more than 15 mm, and that vault over the corneal apex and limbus. They land softly on the conjunctiva without blanching any of its blood vessels. ScCLs provide better visual performance and greater comfort to patients with various ocular surface disorders. They are more comfortable than RGP lenses because their edges don’t interact as much with the eyelids and they are more stable and cantered. ScCLs are indicated in advanced keratoconus or if the patient has failed with previous lens designs, soft or corneal gas permeable, due to discomfort, poor fit, or poor vision.
Advances in the manufacturing of ScCLs allow for correction of both lenticular and/or corneal astigmatism. Front surface toricity to be added to correct residual lenticular astigmatism and for toric peripheral curves to be made if there is significant scleral toricity. One of the most important aspects of fitting is aligning the lens to the sclera to prevent compression, decrease fogging, and promote tear exchange. Toric peripheral curves can be beneficial when fitting ScCLs, as the sclera tends to increase in toricity as its distance from the limbus increases. In addition, correction for front surface eccentricity or wavefront aberration can be added to these lenses in the presence of higher-order aberrations. Some ScCLs feature quadrant-specific peripheral designs that address scleral asymmetry.
Because ScCLs vault over the cornea, they can delay corneal transplants in eyes with minimal central scarring. In 1 study, 40 of 51 eyes with severe keratoconus were successfully treated with ScCLs and spared transplantation. Although this is partly due to the introduction of CXL, ScCLs reduce the lens intolerance and corneal scarring that may have indicated the need for corneal transplant surgery in the past.
Ultimately, 10% to 20% of patients with keratoconus will need some type of corneal transplant. Corneal grafts are indicated in those who cannot tolerate lenses, have significant corneal scarring, are at risk of corneal perforation, or exhibit pronounced corneal thinning or protrusion that inhibits their ability to wear lenses.
Penetrating keratoplasty (PK) removes the entirety of the cornea and replaces it with donor tissue. Deep anterior lamellar keratoplasty (DALK) removes the epithelium and stroma, leaving Descemet’s membrane and endothelium intact and thus helping to maintain ocular integrity, eliminate risk of endothelial cell rejection, and prolong graft life. Although DALK offers faster recovery and visual improvement, patients who undergo PK may achieve better visual acuity in the long run.
Keratoconus Prevalence
Improvements in corneal imaging and mapping technology have dramatically improved eye care professionals’ ability to detect KC, particularly in the early stages of the disease. This is an important development, as the non-keratoplasty treatment for KC, CXL, typically only arrests disease progression, meaning that loss of vision before the intervention tends to remain lost, underscoring the importance of early screening and treatment. As KC prevalence in some populations can be as high as 5%, the importance of identifying and treating this disease early is clear.
Etiology, Pathophysiology, Genetics, and Associated Disease
Through novel genomic testing, more positive associations between various risk factors and genes will be connected to KC. Subsequently, our understanding of associated pathways (i.e. extracellular matrix [ECM]/collagen/cell differentiation) and syndromes (i.e. Down syndrome) will continue to grow and can be utilized to expand future polygenic screening to include more genes/ variants as well. As our foundation of KC genetics expands, key clinical applications such as genetic risk tests may be electively integrated into clinical practice to assist in risk stratification prior to refractive surgery, or for an adjunct to clinical decision making when considering CXL. e potential for developing predictive models for risk percentage thresholds toward guidelines for use in clinical practice leaves room for enormous growth in intertwining genomic advancements with KC management
Corneal Biomechanics and Its Relationship to Keratoconus
The refractive performance of the eye is determined to a
large extent by the corneal shape, which is governed by its mechanical
properties and tissue microstructure. The origin of these structural and
functional alterations in keratoconus (KC) is still controversial but most
likely contains a genetic and environmental component. While in diseases such
as Trisomy 21, Leber’s congenital amaurosis, Ehler-Danlos syndrome, and
osteogenesis imperfecta, an increased susceptibility to contract KC has been
reported, there is no clear pattern of inheritance for KC. Still, a predisposition
to an abnormal collagen metabolism seems to favour mechanical destabilization
and thus the incidence of the disease. At the same time, eye rubbing is an
acknowledged risk factor for KC. It appears to not directly mechanically weaken
the tissue but rather to trigger an inflammatory reaction stimulating an
excessive degradation of the extracellular matrix. In agreement with recent biochemical
analyses in tear film, inflammation is considered the driver of collagen loss
and geometrical degradation in KC.
A convincing advantage of non-contact biomechanical assessment is its comfortability for the patient and easy clinical integration. Yet these approaches come with the challenge of a more complex data interpretation and with the several confounders that can bias the measurement
Optics of Keratoconus and Correcting Aberrations with Wavefront-Guided Lenses
'Similar to a mythical unicorn, contact lenses with wavefront-guided optics was something people liked to talk about, but nobody had ever seen.
A soft lens version became available, but the results were not what was needed for our patients. So what about doing a wavefront-guided surface on a Scleral lens?'
Customization of corrections for the population of individuals with KC is emerging, but much work is left to do before these lenses are commonplace. Additional scientific understanding of how the human visual system perceives the improved visual quality, and engineering developments to stabilize the lenses on-eye without affecting ocular health, are needed. These endeavours will perhaps motivate all of us to move toward a more complete form of correction for this segment of the population, with the result that the KC group is seen as not so “challenging” or “demanding” over all. Truth be told, what the KC population is really asking for as a whole is simply to have a level of corrected visual performance that the typical myope and hyperope might currently take for granted.
Diagnostics and Monitoring
Keratoconus is a progressive disease that can negatively impact a patient’s visual function and overall quality of life. With the advent of highly sensitive and specific advanced diagnostic technologies, along with our ability to halt the progression of the disease with CXL, we now have the opportunity to preserve our patients’ vision. Modern management relies on diagnosing KC as early as possible and monitoring for any evidence of progression. Should we detect progression or diagnose patients who are at high risk for progression, consideration of CXL must be made.
Paediatrics and Keratoconus
In giving particular attention, early detection and treatment is paramount to avoid serious visual impairment. Corneal crosslinking offers a true treatment for KC, halting the corneal changes and avoiding the gamut of visual rehabilitation options. Paediatric patients with KC require early diagnosis, careful examination, and early intervention by CXL to ensure a positive visual prognosis and to avert vision loss.
Corneal Crosslinking for Keratoconus and Corneal Ectasia
It needs to be emphasized that that there are ever evolving optimizations of CXL taking place. As such, there are several modifications to the original FDA-approved CXL procedure that are currently under investigation and a FDA approved Epi On procedure that is being deployed. Transepithelial CXL, in particular, is a variation of the standard procedure in which the corneal epithelium is not removed. This technique may offer several advantages, including faster recovery time and fewer wound-healing complications. However, early results of transepithelial CXL have been mixed. Multiple substances, such as benzalkonium chloride, EDTA, and sodium iodide have been used to promote riboflavin penetration through the epithelium and improve the actual crosslinking reactions.
Additionally, iontophoresis and additional corneal oxygenation have been used; the former to improve the penetration of riboavin, and the latter to improve oxygen-dependent CXL reactions with the goal of improving transepithelial CXL outcomes. In addition to the riboflavin used for transepithelial CXL, modications to the standard dextran riboflavin used for traditional CXL have also been made. Standard dextran riboflavin has a dehydrating effect on the corneal stroma, and frequently hypotonic riboflavin is required to swell the cornea before UV light therapy is initiated. Hypotonic forms of riboflavin, methylcellulose riboflavin, and more concentrated versions of riboflavin have all been studied.
Early studies appear to indicate that CXL
is successful in conjunction with most of these riboflavin formulations;
however, long-term and prospective studies are required to determine the
optimal riboflavin composition for transepithelial CXL. Further medication’s to
the CXL procedure have been suggested for thin corneas. In the FDA trial, the
cornea was required to be thicker than 400 µm to perform CXL treatment. In
addition to the alternative forms of hypotonic riboflavin and the
transepithelial CXL approach discussed above, further modifications such as
contact lens or lenticule-assisted CXL can be considered. In both cases, the
epithelium is removed from the patient’s cornea, and either a contact lens
soaked in riboflavin or a corneal lenticule preserved from a previous SMILE
procedure are used to cover the patient’s cornea and modulate the depth of the
CXL in the patient’s stroma. Finally, algorithms are being developed to
optimize the time of UVA light exposure (less than the standard 30 minutes) to
customize the depth of CXL treatment, depending on the corneal thickness.
Practice Considerations in Managing Keratoconus and Cross-Linking
Scleral lens fittings and the management of progressive KC patients who are undergoing cross-linking are among the most rewarding things an optometrist can get involved in. First and foremost, you are offering a treatment that treats progression. Furthermore, patients are so very appreciative when you can pinpoint the cause of and address their visual quality problems with contact lenses. Modelling suggests that iLink® cross-linking saves the average patient nearly $9,000 in direct medical costs and nearly $44,000 in lifetime costs - and that doesn’t even include the impact on their mental health and well-being. In addition to the cost savings, it is very fulfilling to me to know you can help protect a young person with early progressive KC from progressing to the advanced stages of the disease, potentially avoiding a lifetime of vision loss and the need for corneal transplant surgery. Studies show a 25% drop in corneal transplants after the introduction of cross-linking. Our KC patients are grateful for this care. They will rave about you on social media, refer family and friends—and generally become loyal patients.
KEY TAKEAWAYS
- Cross-linking, in the US is the only FDA-approved system that can treat progressive Keratoconus.
- With Crosslinking 26% fewer Penetrating Keratoplasty, 28 fewer years in late-stage KC.
- Early diagnosis and treatment are essential to preserve as much vision as possible.
- Optometrists are uniquely positioned to change lives and protect vision by identifying at-risk patients in the mild stages of the disease.
The ability to stabilize the cornea with CXL has created the opportunity to surgically improve corneal topography/tomography and both corrected and uncorrected visual acuity. Many of these patients can benefit from the ability to wear spectacles for more functional vision after topography-altering surgery.
While the original Dresden protocol laid a solid foundation, the field is moving towards more sophisticated approaches that integrate technological advances, an improved understanding of corneal biomechanics, and patient-specific customization. These developments not only enhance the scope of CXL but also underline the importance of ongoing research to refine and expand its applications in corneal pathology.
A specialty contact lens may be fit to achieve best corrected visual acuity, and these patients can choose to wear spectacles during times of less visual demand. This may decrease contact lens intolerance and preserve the ability to wear specialty contact lenses for times of higher visual demand throughout their lives. Additionally, diagnosing KC early remains critical to stabilize the cornea prior to disease progression. Modern surgical treatments can then be performed to improve corneal topography and both uncorrected and corrected vision. When necessary, modern technology has also improved corneal transplantation, in particular, deep anterior lamellar keratoplasty procedures. New surgical procedures, such as corneal tissue derived intracorneal ring segments, may offer the opportunity to treat patients with a more customized, topography-altering surgical treatment for improved visual correction in KC.
Specialty Contact Lenses for Keratoconus
Advancements in managing ectatic corneal diseases offer a variety of tailored contact lens options. Personalized fitting, including scleral lenses, is crucial for optimal outcomes by improving vision and addressing high-order aberrations associated with these conditions. As our understanding of ectatic corneal diseases continues to evolve, it is vital for eye care practitioners to stay updated with the latest developments and provide personalized solutions for the best possible care of patients with these complex conditions.
Specialty CL prescriptions are not simply placing a piece of plastic on an eye. They are used as part of the comprehensive management of ocular pathology. On-going evaluation of the health and integrity of the ocular surface is essential. Technology has improved our understanding of ocular surface contour and has improved our ability to manufacture lenses that more closely align to that contour to provide good vision and comfort while maintaining ocular health.
Collaborative Care in Keratoconus
Ectatic corneal diseases - such as keratoconus - pose significant challenges to vision and quality of life, professionals have become dedicated to better understanding the underlying causes and advancements in treatment methods for its successful management.
With a multidisciplinary approach that includes early diagnosis, monitoring, patient education, and advancements in contact lenses and surgeries, professionals can offer better visual outcomes and significantly improve the quality of life for patients affected by ectatic corneal diseases.
Prompt diagnosis and regular monitoring are essential for successful outcomes with corneal crosslinking in halting the progression of keratoconus. Additionally, educating patients about the significance of avoiding eye rubbing is crucial for preventing and managing the disease effectively.
If the KC management protocol follows the steps of an early diagnosis, halting disease progression, and optimizing visual quality, then a collaborative care model fits beautifully. We see this collaborative care model as a win-win-win. It is a win for optometrists because they can concentrate on being excellent diagnosticians and rehabilitating the ectatic eye with spectacle and contact lens devices. It is a win for surgically oriented practices, as they can see more patients that need specialized care. Most importantly, the patient wins because collaborative care with excellent communication and an interventional mindset in KC aims to preserve visual quality and, in many cases, improve acuity, and in turn, quality of life. Read more...
Test. Treat. Track.
In Summary
A number of options exist for managing the various stages of keratoconus. At diagnosis - or at first sign of progression - young patients should be referred for an evaluation for CXL. Patients who previously worse lenses will most likely require post-procedure refitting after CXL. The severity of the condition may dictate the type of lens used: soft, specialty soft, hybrid, piggyback, RGP, or ScCL. When the patient can no longer tolerate lenses and tissue-sparing surgery options are not possible or there is significant corneal scarring, a corneal transplant then becomes an option (corneas being the most frequently transplanted organ), be it DALK or PK. Even after partial or total transplantation, patients can continue to be co-managed and may still require contact lenses.
All content is intended for informational series and should not be used as a substitute for medical advice.











.png)
![[Video] Adverse Eye Rubbing in Keratoconus](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEg4HRiK6MvFtia856foWYkBDP2bCVe0NB-S445VtbzLVYY19KJ6Pma-J-xabIQgjfE3RyTgr5C7Y9IvGs6PZ2ofcR13vtnGSwqghFJv40mZdjUD4VyOfjGN03Fhyphenhyphenziai2VNOASlDExTi77TdfDrh2yKeS735QlfIwwLZhn0xilsHeLiGDvhshth384ZzgBu/w72-h72-p-k-no-nu/keratoconus-pathogenesis.jpg)

